Implantable Devices for Pain Relief
PORTS
I have posted previously in the My Journal page about I.V. Access Devices, or as they are more commonly referred, ports. However, I felt that this was something that deserved more attention. Most LPHS patients are frequent visitors to the hospital, where we require I.V. pain meds, nausea meds and various fluids. The longer we suffer from the illness, the more wear and tear our veins receive. Especially if you have bad veins like I do, it becomes increasingly difficult to find viable veins for I.V. access.
In October of 2012, more than two years into my illness, I had the procedure to have a port implanted. It was one of the best decisions I have ever made. It greatly simplifies the prep time in the Emergency Room and drastically reduces the pain I had been subjected to due to numerous needle sticks. The picture to the right is of me in the hospital with my port accessed.
What is a port, exactly?
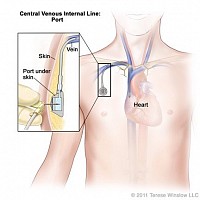
A port is a device for intravenous access in patients who require frequent or continuous administration of intravenous substances. Implantation is typically an outpatient procedure, done with local anesthetics and possible conscious sedation. An interventional radiologist will use x-rays and ultrasound equipment to properly place the device before making the 1-2 inch incision in the chest, just below the clavicle. The device consists of a plastic tube, which is placed into one of the larger arteries close to the heart, and a chamber connected to the tube. The chamber has a silicone membrane that can be accessed by puncturing the overlying skin with a Huber point needle, and fluids can be injected.
Can blood be drawn from the port?
Yes. Blood may be drawn from the port for labs or other tests. Sometimes a port will "flush", meaning that fluids can be injected, but there may not be a blood return. There are many reasons why this may happen. First, have the nurse flush the line with Heparin, a blood thinning medication that will dissolve any possible blood clots. (Ports are almost always flushed with Heparin when they are accessed and de-accessed.) Second, it may simply be the way your body is positioned. Try changing positions, sitting upright, moving the arm closest to the port, or sometimes coughing may do the trick. If you are still having difficulty getting a blood return, you may need to make an appointment with your Infusion clinic to have them check it out.
How long do ports last before they need to be replaced?
Some sources say anywhere from 2-6 years. However, there are patients who have had their devices for almost 10 years and they are still functioning normally. If your device is not accessed regularly, you should go to your Infusion clinic to have it flushed every 4-6 weeks. This will keep it flushing smoothly and give your device the best lifespan possible. Chest ports typically withstand approximately 2,000 punctures.
What is the difference between a regular port and a PowerPort™?
PowerPort™ is a specific brand that has the capability of allowing power injection of contrast media for CECT (Contrast Enhanced Computer Tomography) scans. The high rate of injection allows for more detailed images to be captured for the purpose of tracking tumor markers or pulmonary embolisms. It also performs the same functions of any other port, injection of medications and blood return.
Are all regular ports the same?
For the most part, yes, but there can be some minor differences. The majority of the ports you will see are "single lumen" ports, meaning that there is one silicone membrane for attachment to the plastic intervascular tube. However, there are some "double-lumen" ports that have two silicone membranes.
What is the difference between an Arm port and a Chest Port?
Arm ports are typically lower profile and smaller. Because of their smaller size, arm ports are usually good for approximately 1,000 punctures while chest ports roughly 2,000 punctures.
Benefits of an Arm port:
- Arm port advocates cite a forearm skin bacteria count 100 - 1000 times less than the chest, which would indicate a lower infection rate.
- Arm ports are smaller, less visible and easier to conceal under clothing.
- It is closer to the jugular and subclavian veins and therefore requires less tubing.
- It allows for twice the number of punctures of Arm ports.
*Update*
Shortly after posting the information on this page, I went through a pain flare and had to be admitted to the hospital. During my stay, my port was flushing but not giving a blood return. The nurses did a couple of rounds of medication, hoping to unblock the port and be able to draw blood for my labs. However, the attempts were unsuccessful. They sent me down to Interventional Radiology to have the port examined and to determine the appropriate course of action. The doctors injected some contrast material and did some imaging tests. They determined that the best thing would be to replace the port completely. As I had already had the port nearly five years, it was toward the end of its' life expectancy. The doctors removed the old port, which had been on the left side of my chest, and placed a new PowerPort on the right side of my chest. They accessed the new port and it worked like a dream! It has now been about three weeks since the surgery and I am almost completely healed.
To the left is a picture of my old port after it was removed. I asked if I could have it, and they cleaned it up for me. I wanted to be able to show my family and also share pictures here, to better explain ports and show what they look like.
PAIN PUMPS
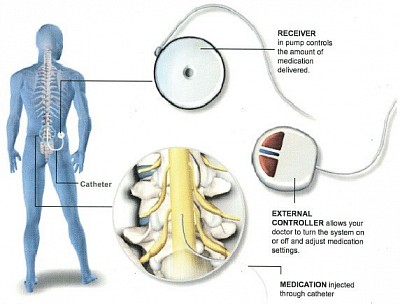
An intrathecal pain pump is a small medical device, that delivers medications directly to the spinal cord, into the fluid that surrounds the cord itself. Medications placed here have a stronger and faster pain relief effect than medications taken in pill form. Additionally, less medication is required as it is going directly to one of the main pain centers in the body. According to treatingpain.com, the website of National Spine and Pain Centers, “The spinal cord is the “mecca” of pain sensations. Just like the brain, the spinal cord is very important in receiving pain signals from the rest of the body. It has many receptors (sensors), that can shut off the pain. Among these are the opioid receptors. Opioids are commonly used in pain pumps, sometimes in combination with other medications. When delivered through a pain pump, opioids have fewer systemic (body-wide) side effects. A pain pump is a great way to control long-lasting pain that has failed to improve with other treatments or with surgery.”
Advantages of Pain Pumps:
- Only a small amount of medication is needed - Medications taken in pill form must travel throughout the body before reaching the spinal cord. Roughly 1/300th of the dose of the pill form medication is needed to give relief via a pain pump, as it is going directly where it is needed.
- Fewer side effects - Giving medications through a pain pump reduces side effects such as nausea, constipation and drowsiness.
- Reduced risk of addiction - As a much smaller dose is required to be effective, there is a reduced risk of addiction to the opioid medications frequently used in pain pumps.
- No need to remember to take your medication - Pain pumps release medications slowly and constantly. They can also be programmed to give you extra medication during the time of day when your pain may be worse. There is also no need to fill a monthly prescription. Your doctor’s office will refill the pump every 3-6 months.
To determine if a pump would be a good option for a patient, the pain management doctor will do a trial which consists of giving a shot of medication into the fluid around the spinal cord. If the patient’s pain is reduced by at least 50%, the trial is deemed successful and the patient is scheduled to have the pump implanted.
The procedure to implant the pump is done under general anesthesia, meaning that they will put you to sleep. The entire procedure takes approximately 30 minutes to an hour.
The National Spine and Pain Centers’ website states that there are three main steps to the procedure:
- A catheter (thin tube that delivers medication) is placed in your back (spinal space).
- The pump (reservoir that holds and delivers medicine) is placed under the skin of your abdomen, below the waistline. This placement is comfortable for you and unlikely to show through your clothes.
- Medication flow is started once the catheter is connected to the pump.